How to Lower Diastolic Blood Pressure
Diastolic blood pressure refers to the pressure in your arteries when your heart relaxes between beats. This is the lower number in a blood pressure reading for example, in 120/80 mmHg, the “80” represents diastolic pressure. This measurement reflects how much resistance your blood vessels offer when the heart is at rest, and it plays a vital role in overall heart health.
Managing diastolic blood pressure is crucial because consistent high levels indicate that your arteries are not relaxing properly, putting extra strain on your heart and circulatory system. Over time, high diastolic blood pressure can cause serious health risks such as heart disease, stroke, and chronic kidney damage. Even if the systolic pressure (the top number) is normal, elevated diastolic pressure alone can silently damage your blood vessels and organs.
On the other hand, lowering diastolic blood pressure to a healthy range improves blood flow, reduces stress on the heart, and helps prevent complications. Through lifestyle changes such as better nutrition, regular physical activity, stress management, and proper medical care, you can support long-term cardiovascular resilience and overall well-being.
What Is Diastolic Blood Pressure?
During the relaxation phase of your heartbeat, your heart refills with blood while your arteries maintain enough tension to keep blood flowing smoothly throughout your body. This value shows how flexible and healthy your arteries are when they’re not under the direct force of a heartbeat. This is what is known as Diastolic blood pressure.
Diastolic blood pressure is different from systolic blood pressure, which measures the pressure in your arteries when the heart contracts and pumps blood out. Let’s review a reading like 120/80 mmHg, here the top number (120) is the systolic pressure, and the bottom number (80) is the diastolic pressure. Measuring is usually done using a blood pressure cuff (either manual with a stethoscope or digital). The cuff inflates around your upper arm to temporarily stop blood flow, then slowly releases pressure while detecting the sounds or vibrations of blood moving through your arteries.
Normal diastolic blood pressure typically falls between 60 and 80 mmHg. Readings consistently above 80 mmHg may indicate elevated or high blood pressure, while those below 60 mmHg can suggest low blood pressure, which might also cause symptoms such as dizziness or fatigue.
Why Is It Important to Lower Diastolic Blood Pressure?
It is ideal to maintain your diastolic blood pressure within a healthy range. This is essential for protecting your heart, blood vessels, organs and overall longevity. When the diastolic pressure stays high, it causes your arteries remain under constant strain even when your heart is resting. Over time, this persistent pressure can cause silent yet serious damage to vital organs, such as tour heart, kidneys, and blood vessels.
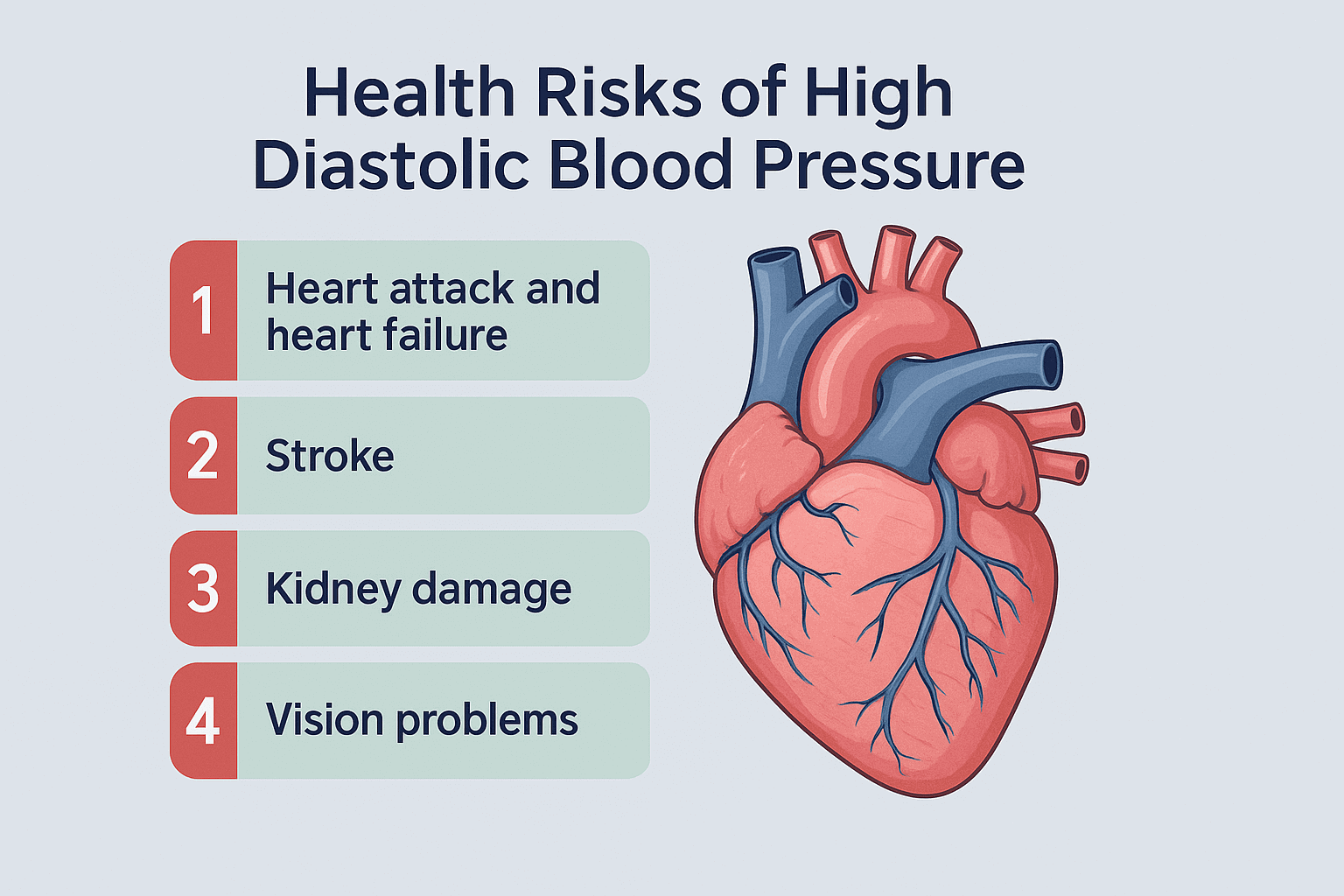
Health Risks of High Diastolic Blood Pressure
Chronic elevation of diastolic pressure can lead to several long-term complications, including:
Heart attack and heart failure: High diastolic pressure forces your heart to work harder, thickening the heart muscle and reducing its efficiency over time.
Stroke: Constant pressure damages arterial walls, making them more likely to rupture or form clots that block blood flow to the brain.
Kidney damage: The kidneys depend on stable blood flow to filter waste; high diastolic pressure can harm these delicate vessels, leading to kidney disease or failure.
Vision problems: Increased pressure may affect small blood vessels in the eyes, contributing to retinal damage or vision loss.
Importance of Early Detection and Control
High diastolic blood pressure, also known as the silent killer, often develops gradually and without obvious symptoms. Regular monitoring, lifestyle changes, stress reduction, proper diet and exercise and, if needed, medication can help bring reading back to a safe range.
Impact on Heart Health and Longevity
Lowering diastolic blood pressure reduces strain on your cardiovascular system, improving circulation and allowing your heart to rest more efficiently between beats. Over time, maintaining a healthy diastolic range supports stronger arteries, reduced risk of chronic disease, and longer life expectancy.
How to Lower Diastolic Blood Pressure
Managing diastolic blood pressure effectively involves a blend of lifestyle changes, medical guidance, and consistent monitoring
Lifestyle Approaches to Lower Diastolic Pressure
Heart healthy diet is essential
Focus on nutrient-rich foods like fruits, vegetables, whole grains, lean proteins, and healthy fats.
Limit sodium intake (ideally under 1,500 mg per day) to help reduce water retention and blood vessel strain.
Choose potassium-rich foods (bananas, sweet potatoes, spinach) to balance electrolytes and ease vascular tension.
The DASH diet (Dietary Approaches to Stop Hypertension) is a proven method to lower both systolic and diastolic pressure naturally.
Regular exercise and mobility
Engage in at least 150 minutes of moderate aerobic activity per week, such as brisk walking, cycling, or swimming.
Incorporate strength training and flexibility exercises to improve circulation and reduce overall stress levels.
Stress management
Chronic stress can elevate diastolic pressure. Practice deep breathing, yoga, meditation, or tai chi.
Prioritize rest, relaxation, and social support to help your body reset its natural blood pressure rhythm.
Limit Alcohol, Caffeine, and Tobacco
Excessive alcohol and caffeine can temporarily raise blood pressure.
Avoid smoking, as it stiffens arteries and accelerates blood vessel damage.
Maintain Healthy Weight
Even a small weight loss (5–10 pounds) can significantly reduce diastolic readings.
Medical and Supplement Support
Lowering the bottom number of your blood pressure reading not only reduces cardiovascular risks but also supports long-term heart and kidney health. But if lifestyle changes alone don’t bring your numbers to a normal healthy range, your healthcare provider may recommend other alternatives:
Prescription medications such as ACE inhibitors, beta-blockers, or calcium channel blockers to relax blood vessels.
Natural supplements like magnesium, omega-3 fatty acids, or CoQ10 (under provider supervision) to support vascular health.
Set Realistic Blood Pressure Goals
An ideal blood pressure reading is around 120/80 mmHg, but not every individual is going to have the same goals. These goals may vary based per individual and on age, health conditions, and medications. Your provider is here to help you to establish a personalized target range and create a gradual plan to achieve it safely.
Foods to Eat and Avoid for Reducing Diastolic Blood Pressure
A balanced, heart-focused diet is one of the most effective natural tools for lowering blood pressure and supporting long-term cardiovascular health.
DASH diet (Dietary Approaches to Stop Hypertension) which emphasizes fruits, vegetables, whole grains, and low sodium has been clinically proven to lower both systolic and diastolic blood pressure.
Foods That Help Lower Diastolic Blood Pressure
Fruits and Vegetables
Leafy greens (spinach, kale, Swiss chard): high in potassium, which helps flush out sodium.
Berries (blueberries, strawberries): packed with antioxidants that protect blood vessels.
Citrus fruits (oranges, grapefruits, lemons): support healthy artery function with vitamin C and flavonoids.
Bananas: a top source of potassium to balance sodium levels naturally.
Beets: rich in nitrates that help widen blood vessels and lower diastolic pressure.
Whole Grains
Oats, quinoa, brown rice, and whole-wheat bread improve circulation and reduce cholesterol buildup.
Fiber-rich grains stabilize blood sugar and support heart health.
Lean Proteins and Healthy Fats
Fish (salmon, mackerel, sardines): provide omega-3 fatty acids that reduce arterial inflammation.
Nuts and seeds (almonds, flaxseeds, chia seeds): offer magnesium and healthy fats that relax blood vessels.
Legumes (lentils, chickpeas, beans): plant-based proteins that promote vascular health.
Olive oil and avocado: heart-healthy fats that improve cholesterol and lower blood pressure naturally.
Low-Fat Dairy and Dark Chocolate (in moderation)
Calcium-rich dairy products can help regulate blood pressure.
Dark chocolate (70% or higher) contains flavonoids that improve vessel elasticity.
Foods and Substances to Avoid
Processed and Packaged Foods
Often loaded with sodium, trans fats, and preservatives that raise blood pressure.
Examples: frozen dinners, canned soups, deli meats, chips, and fast food.
Salty Foods
Excess salt causes your body to retain fluid, increasing arterial pressure.
Aim for less than 1,500 mg of sodium per day.
Sugary and Refined Foods
Added sugars, pastries, and sodas contribute to weight gain and insulin resistance, which can raise blood pressure.
Caffeinated and Alcoholic Beverages
Too much caffeine can temporarily spike blood pressure.
Limit alcohol to no more than one drink per day for women and two for men to protect heart health.
Exercise Recommendations for Lowering Diastolic Blood Pressure
Regular physical activity is one of the most effective and natural ways to lower diastolic blood pressure and improve overall cardiovascular health. Consistent physical activity not only helps lower diastolic blood pressure but also supports healthier weight, reduces stress, and boosts overall well-being key ingredients for lasting heart health.
Types of Exercises That Help Lower Diastolic Blood Pressure
Aerobic (Cardio) Exercise
Activities like brisk walking, cycling, swimming, or dancing are ideal for improving heart health and lowering both systolic and diastolic pressure.
Aim for at least 150 minutes per week of moderate-intensity cardio or 75 minutes of vigorous activity.
Even short 10–15-minute walks after meals can significantly help regulate blood pressure.
Strength Training
Incorporate 2–3 sessions per week of light to moderate resistance training using body weight, resistance bands, or light dumbbells.
Focus on large muscle groups (legs, back, chest) with controlled breathing—exhale during exertion to prevent sudden spikes in pressure.
Flexibility and Balance Exercises
Activities like yoga, Pilates, or stretching promote relaxation, improve circulation, and reduce stress hormones that elevate blood pressure.
Gentle stretching after workouts or before bed supports recovery and vascular health.
Isometric Exercises (Static Holds)
Simple isometric moves—like wall sits or plank holds—can improve vascular strength and lower resting diastolic pressure when done correctly and safely.
Perform short sets (15–30 seconds) and breathe normally throughout to avoid pressure surges.
Tips for Safe Exercise with High Blood Pressure
Consult your healthcare provider before starting or changing an exercise routine, especially if your blood pressure is high or uncontrolled.
Warm up and cool down for at least 5–10 minutes to ease your heart rate in and out of activity.
Avoid heavy lifting or breath-holding, as these can cause dangerous spikes in blood pressure.
Stay hydrated and avoid exercising in extreme heat or cold, which can stress your cardiovascular system.
Monitor your heart rate and symptoms—stop immediately if you feel dizzy, lightheaded, or unusually short of breath.
How Losing Weight Helps Lower Diastolic Blood Pressure
Weight management plays a vital role in controlling diastolic blood pressure and protecting heart health. Even modest weight loss can significantly improve how efficiently your heart pumps blood and how well your arteries relax between beats.
There is a Relationship Between Obesity and High Blood Pressure
When you carry excess body weight especially around the abdomen, It places extra strain on your heart and blood vessels. This additional pressure causes your heart to work harder to circulate blood, which can raise both systolic and diastolic blood pressure over time.
Obesity also contributes to other physiological changes that worsen hypertension, such as:
Insulin resistance, which disrupts how your body regulates blood sugar and sodium balance.
Inflammation and oxidative stress, which damage artery walls and reduce elasticity.
Increased blood volume, which leads to higher resting pressure in the arteries.
Studies show that for every 5–10 pounds lost, many people experience noticeable improvements in both diastolic and systolic readings—sometimes by as much as 5–10 mmHg.
Practical Weight Loss Strategies to Improve Blood Pressure
Adopt a Balanced, Low-Sodium Diet
Follow the DASH or Mediterranean diet, focusing on vegetables, fruits, lean proteins, and whole grains.
Reduce added sugars and processed foods to decrease caloric intake and prevent fluid retention.
Increase Daily Physical Activity
Combine aerobic workouts (like walking or cycling) with strength training to boost metabolism and fat loss.
Incorporate movement into your day—take stairs, stretch breaks, or evening walks.
Monitor Portion Sizes and Eat Mindfully
Slow, intentional eating helps prevent overeating and improves digestion.
Use smaller plates and measure portions to maintain calorie awareness.
Manage Stress and Sleep
Chronic stress and poor sleep can trigger hormonal imbalances that hinder weight loss and raise blood pressure.
Aim for 7–9 hours of sleep per night and practice relaxation techniques like deep breathing or meditation.
Set Realistic Goals (remember this lifestyle change will not happen overnight)
Aim to lose 1–2 pounds per week for sustainable results.
Remember, even gradual weight loss can produce meaningful drops in blood pressure and reduce cardiovascular risks.
Natural Supplements and Herbs That Can Lower Diastolic Blood Pressure
In addition to healthy lifestyle changes, certain natural supplements and herbs have been shown to support healthy blood pressure levels especially when used under professional guidance.
Scientifically Supported Supplements
Magnesium
How it helps: Magnesium relaxes blood vessels and supports normal muscle and nerve function, helping to reduce arterial tension.
Sources: Leafy greens, nuts, seeds, and whole grains—or supplements such as magnesium glycinate or citrate.
Guidelines: Adults generally need 300–400 mg daily. Too much can cause diarrhea or low blood pressure, so consult your provider before use.
Omega-3 Fatty Acids (Fish Oil)
How it helps: Found in fish like salmon and sardines, omega-3s lower triglycerides, reduce inflammation, and improve arterial elasticity.
Guidelines: Typical dosage ranges from 1,000–3,000 mg of combined EPA and DHA daily. Choose purified supplements to avoid heavy metal contamination.
Garlic Extract
How it helps: Garlic promotes nitric oxide production, which relaxes blood vessels and improves circulation. Studies have shown it can lower both systolic and diastolic pressure.
Guidelines: Aged garlic extract (600–1,200 mg daily) is well-tolerated and effective. Raw garlic can also be added to meals for additional benefits.
Hibiscus Tea
How it helps: Hibiscus is rich in anthocyanins and antioxidants that help dilate blood vessels and reduce arterial stiffness.
Guidelines: Drinking 1–2 cups daily can help modestly reduce diastolic blood pressure over time. Avoid if you take diuretics or blood pressure medications unless advised by a clinician.
Additional Herbal Remedies and Nutrients
CoQ10 (Coenzyme Q10): Supports heart energy production and has mild blood pressure lowering effects (100–200 mg daily).
Beetroot Powder or Juice: Contains natural nitrates that improve blood vessel dilation.
Potassium: Helps balance sodium levels in the body—best obtained through food rather than supplements unless prescribed.
Safety Precautions
Always consult your healthcare provider before adding supplements, especially if you take prescription medications for hypertension, diabetes, or heart disease.
Choose high-quality, third-party tested products to ensure purity and potency.
Avoid mixing multiple blood pressure lowering supplements without supervision, as this can cause excessive drops in blood pressure.
Pregnant or breastfeeding individuals should use herbal remedies only under medical advice.
Used correctly, natural supplements and herbs can complement your lifestyle and medical plan, helping you manage diastolic blood pressure safely and effectively over time.
Managing Stress and Improving Sleep to Control Diastolic Blood Pressure
Chronic stress and poor sleep are two major yet often overlooked contributors to high diastolic blood pressure.
Stress Reduction Techniques for Healthy Blood Pressure
Meditation and Mindfulness
Practicing meditation for even 10–15 minutes daily helps calm the nervous system and lower cortisol levels.
Techniques like guided meditation or mindful breathing focus your attention on the present moment, reducing anxiety and blood vessel constriction.
Deep Breathing Exercises
Slow, controlled breathing (such as the 4-7-8 technique) activates the parasympathetic nervous system the body’s natural relaxation response.
Try inhaling for 4 seconds, holding for 7 seconds, and exhaling slowly for 8 seconds to lower your heart rate and diastolic pressure.
Progressive Muscle Relaxation
Tensing and relaxing muscle groups from head to toe helps release physical tension and improve circulation.
Especially effective before bedtime to prepare the body for restful sleep.
Yoga and Tai Chi
These gentle movement practices blend deep breathing, stretching, and mindfulness to enhance flexibility, improve blood flow, and reduce stress hormones.
Time in Nature and Hobbies
Spending time outdoors, gardening, or engaging in creative hobbies (like painting or music) helps reset emotional balance and lower blood pressure naturally.
Sleep Hygiene Tips for Blood Pressure Control
Maintain a Consistent Sleep Schedule
Go to bed and wake up at the same time each day even on weekends to regulate your body’s internal clock.
Creating a Relaxing Bedtime Routine is key
Wind down with calm activities like reading, stretching, or listening to soft music. Avoid stimulating screens and bright lights at least 30–60 minutes before bed.
Optimize Your Sleep Environment
Keep your bedroom cool, dark, and quiet.
Invest in a comfortable mattress and pillow to promote deeper, uninterrupted rest.
Limit Stimulants and Alcohol
Reduce caffeine intake after noon and avoid alcohol before bedtime it can disrupt deep sleep cycles and increase overnight blood pressure.
Address Sleep Disorders Early
Conditions like sleep apnea can cause persistent high diastolic pressure. If you snore or feel tired despite sleeping, talk to your provider about screening.
When to Consider Medication vs. Lifestyle Changes for Diastolic Blood Pressure
Managing diastolic blood pressure often begins with lifestyle changes. However, in some cases, medication becomes necessary to bring levels down to a safe range and prevent complications.
When Medication Becomes Necessary
Medication may be required when:
Diastolic blood pressure remains above 90 mmHg even after consistent lifestyle changes.
There is coexisting systolic hypertension (140/90 mmHg or higher).
You have additional risk factors like diabetes, kidney disease, heart disease, or a family history of hypertension.
You experience organ damage symptoms (e.g., chest pain, shortness of breath, vision problems, or swelling in the legs).
Your provider identifies secondary hypertension caused by another medical condition that needs medication management.
In such cases, antihypertensive medications help protect organs, reduce cardiovascular risks, and prevent long-term damage while lifestyle changes continue to provide supportive benefits.
The Ideal Approach: A Combined Plan
In most cases, medication and lifestyle changes work best together. While drugs lower blood pressure more quickly, lifestyle habits provide lasting control and may reduce the need for higher doses or multiple medications over time. Regular follow-ups with your healthcare provider are essential to adjust medications, evaluate progress, and ensure your treatment plan keeps your diastolic blood pressure within a safe and healthy range.
Conclusion
Managing diastolic blood pressure is a crucial part of protecting your heart, brain, and overall health. Elevated diastolic pressure can silently strain your arteries and organs, increasing the risk of heart disease, stroke, and kidney damage over time.
The good news is that by staying aware of your readings, partnering with your healthcare provider, and making small daily improvements, you can take control of your blood pressure and reduce long-term risks. Every healthy choice matter whether it’s a nutritious meal, a walk, or a calm night’s rest moves you closer to lasting diastolic blood pressure management and a stronger, healthier future.
Frequently Asked Questions
-
You can naturally lower your diastolic blood pressure by following a heart-healthy lifestyle. Focus on eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while limiting salt, sugar, and processed foods. Engage in regular exercise such as brisk walking or cycling—at least 30 minutes a day, 5 times a week. Managing stress through mindfulness, meditation, or yoga and improving sleep quality are also key to long-term control.
-
High diastolic blood pressure can be dangerous because it keeps your arteries under constant strain, even when your heart is resting. Over time, this increases the risk of heart attack, stroke, kidney disease, and vascular damage. If left untreated, it can silently harm your organs, so early detection and consistent management are critical.
-
Foods that help lower diastolic pressure include:
Leafy greens (spinach, kale) for potassium
Berries and citrus fruits for antioxidants
Whole grains like oats and quinoa
Fish rich in omega-3 fatty acids
Nuts, seeds, and legumes for magnesium and fiber
Beets and garlic, which promote blood vessel relaxation
Avoid salty, processed, and sugary foods that can raise blood pressure. -
The best exercises include aerobic activities (walking, swimming, cycling), light strength training, yoga, and deep breathing exercises. Aim for regular, moderate-intensity workouts to strengthen your heart and improve circulation. Always warm up, cool down, and check with your provider before starting a new exercise routine—especially if you have hypertension.
-
The timeline varies depending on lifestyle consistency and overall health. With regular exercise, a heart-healthy diet, and stress reduction, you may start seeing results in as little as 2–4 weeks. However, sustained improvement typically occurs over 3–6 months of consistent effort. Medication, when prescribed, can bring faster results but still works best alongside healthy habits.
-
Key changes include:
Reducing sodium intake to less than 1,500 mg daily
Eating more potassium-rich foods
Exercising regularly
Maintaining a healthy weight
Limiting alcohol and caffeine
Quitting smoking
Managing stress and improving sleep quality
Together, these habits help your arteries relax, improve heart efficiency, and promote lasting blood pressure balance.