What are the common symptoms of chronic pain?
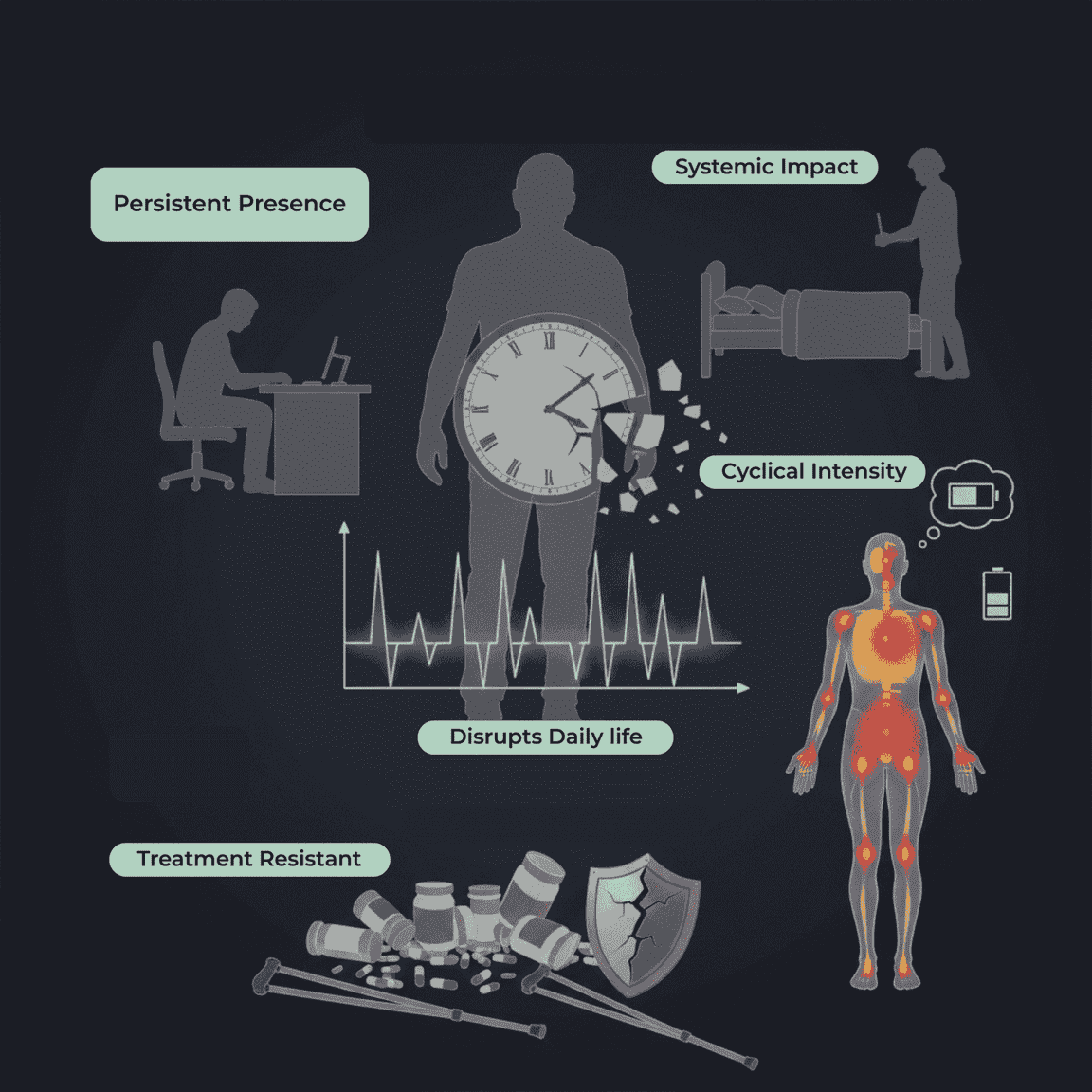
Chronic pain is persistent discomfort that lasts longer than three months, often continuing even after the original injury or condition has resolved. Unlike acute pain, which is short-term and protective, chronic pain can linger for months or years and may fluctuate in intensity. It can affect nearly every part of daily life from sleep and mood to mobility and overall wellbeing.
Common symptoms of chronic pain include ongoing aches, sharp or burning sensations, stiffness, fatigue, and increased sensitivity to touch or movement. Many people also experience related issues such as sleep disturbances, reduced range of motion, mood changes, and difficulty performing routine activities. Because chronic pain affects both the body and mind, early evaluation and personalized management are essential for long-term relief and improved quality of life.
How Can I Recognize If My Pain Is Chronic?
If you’ve been wondering whether your discomfort is more than just a temporary issue, you’re not alone and simply asking the question is an empowering first step toward getting the right help. Many people suffer from chronic pain and don’t even know it. Recognizing chronic pain early allows you to seek proper evaluation, prevent worsening symptoms, and reclaim control over your daily life.
Chronic pain isn’t defined by duration alone. While pain lasting more than three months is a key indicator, the pattern, frequency, and impact of your symptoms matter just as much. You may be experiencing chronic pain if your discomfort:
Returns frequently or never fully goes away, even on “good days.”
Interrupts daily activities, such as work, sleep, exercise, or mobility.
Persists despite rest, medication, or previous treatments.
Shifts in intensity, cycling between flare-ups and milder periods.
It is accompanied by fatigue, stiffness, mood changes, or reduced function.
If your pain feels like it’s becoming a long-term companion rather than a temporary inconvenience, it may be chronic and it’s absolutely worth getting evaluated. With the right support, chronic pain can be understood, managed, and significantly improved.
What Types of Pain Sensations Are Typical in Chronic Pain?
Chronic pain doesn’t feel the same for everyone and that’s completely normal. Because long-term pain can come from nerves, muscles, joints, or internal conditions, the sensations vary widely from person to person. Understanding how your pain feels is incredibly important, because accurately describing it helps your healthcare provider pinpoint the cause and choose the most effective treatment.
Here are some of the most common chronic pain sensations and what they may indicate:
Aching or Throbbing: Often linked to muscle tension, arthritis, or inflammation.
Sharp or Stabbing Pain: Can occur with nerve involvement, joint issues, or movement-related injuries.
Burning or Tingling: Frequently associated with nerve damage or neuropathic pain.
Shooting or Radiating Pain: May signal nerve compression, such as sciatic pain.
Stiffness or Tightness: Common in chronic back pain, fibromyalgia, and joint conditions.
Dull, Constant Pressure: Often tied to deep tissues or structural problems.
Hypersensitivity or “Electric” Pain: Suggests overactive nerves or pain pathways.
Many people experience a combination of sensations that shift throughout the day, especially during flare-ups or after certain activities. How precisely you can describe your pain when it happens, how it feels, and what makes it better or worse the faster your clinician can identify the root cause and build a personalized treatment plan.
What Physical Signs Indicate Chronic Pain in the Body?
Chronic pain doesn’t just feel different it often creates visible and measurable changes in the body. These physical signs can help validate your experience, guide diagnosis, and reveal how deeply the pain is affecting your daily life. Recognizing these indicators is an important step toward getting the right care and understanding that chronic pain is a real, physiological condition not “just in your head.”
Here are some of the most common physical signs and secondary effects linked to chronic pain:
Direct Physical Indicators
Persistent tenderness or sensitivity in certain areas
Inflammation, swelling, or warmth around painful joints or tissues
Limited range of motion or difficulty moving a body part
Muscle stiffness or spasms, especially in the back, neck, or shoulders
Changes in posture, such as guarding, leaning, or shifting weight to avoid discomfort
Secondary Physical Effects
Chronic pain also impacts the body indirectly over time:
Muscle weakness or deconditioning from reduced activity
Fatigue and low energy levels caused by constant discomfort
Sleep disturbances, leading to grogginess or slower recovery
Reduced balance or coordination due to altered movement patterns
Headaches or migraines triggered by muscle tension or nerve irritation
Not everyone experiences all of these signs at the same time but a combination of these may be seen at the same time. These signs give healthcare providers valuable clues about how chronic pain is progressing and how it is affecting your overall health. The combination of direct symptoms and secondary changes helps clinicians build a thorough, personalized treatment plan.
How Long Does Pain Have to Last to Be Considered Chronic?
The answer is 3 months.
If you’ve been dealing with ongoing discomfort, you might wonder when pain officially becomes “chronic.” While duration is a key part of the definition, chronic pain isn’t diagnosed only by how long it lasts it’s also about how the pain behaves and how it impacts your daily life.
Medically, pain is considered chronic when it lasts 12 weeks (3 months) or longer. This timeframe is significant because most tissues in the body muscles, bones, ligaments, and skin typically heal within this period. When pain continues beyond the normal healing window, it may signal ongoing inflammation, nerve involvement, or changes in how the brain and nervous system process pain signals.
However, even before the 3-month mark, doctors may suspect chronic pain if:
Your symptoms keep returning in cycles.
Pain persists despite treatment or rest.
The pain is interfering with sleep, mobility, mood, or daily function.
Understanding this timeline helps both patients and clinicians determine when to shift from short-term pain management to a long-term, comprehensive treatment approach.
Can Chronic Pain Cause Symptoms Other Than Physical Pain?
Chronic pain is not just a physical sensation; it’s a whole-body condition that affects multiple systems, often in ways people don’t expect. These secondary symptoms are incredibly common, completely valid, and deeply interconnected with the pain experience. In fact, they can sometimes be as disruptive as the pain itself.
Because chronic pain places ongoing stress on the nervous system, immune system, sleep cycle, and mood-regulating pathways, many people experience additional symptoms such as:
Cognitive and Emotional Symptoms
Brain fog, difficulty concentrating, or slowed thinking
Depression or low mood, often from the constant strain of managing pain
Anxiety, especially around movement, flare-ups, or the fear of worsening symptoms
Irritability or mood swings caused by disrupted sleep or persistent discomfort
Sleep-Related Symptoms
Trouble falling or staying asleep
Non-restorative sleep, where you wake up feeling tired despite sleeping
Heightened pain levels the next day, since poor sleep increases pain sensitivity
Energy and Functional Symptoms
Chronic fatigue, even with minimal physical activity
Reduced motivation, difficulty completing tasks, or slower daily functioning
Sensitivity to touch, noise, or temperature due to an overactive nervous system
Systemic Effects
Digestive issues, such as nausea, constipation, or appetite changes
Headaches or migraines
Muscle tension throughout the body, not just at the original pain site
These symptoms come from the body's attempt to cope with persistent stress and altered pain pathways not from weakness, exaggeration, or imagining the problem. Understanding these broader effects helps patients and healthcare providers create more effective, whole-person treatment plans that support both physical and emotional wellbeing.
When Do Chronic Pain Symptoms Require a Visit to your Provider?
If you’ve been trying to manage your pain on your own but things aren’t improving, it may be time to bring in professional support and there’s absolutely no need to “tough it out.” Chronic pain is a legitimate medical condition and getting help early can prevent symptoms from worsening and improve your quality of life dramatically.
You should consider seeing a healthcare provider when:
Your pain lasts longer than 3 months
Persistent pain that isn’t resolving with time is one of the clearest signs you need a proper evaluation and treatment plan.
Your pain is interfering with daily life
If your discomfort makes it hard to sleep, work, exercise, or care for yourself, it’s time for professional guidance.
Self-management isn’t working
When rest, over-the-counter medications, stretching, or lifestyle changes don’t provide lasting relief, a clinician can uncover deeper causes and offer targeted solutions.
You experience chronic pain warning signs, such as:
Pain that worsens over time
Numbness, tingling, burning, or weakness
Pain accompanied by swelling, redness, fever, or unexplained weight loss
Pain that radiates down the arms or legs
Loss of mobility or function
You’re unsure about the cause of your pain
Your medical provider can perform a full pain assessment, identify patterns, and rule out underlying conditions.
Your pain is affecting your mental or emotional health
Chronic pain often contributes to mood changes, stress, anxiety, or depression are all valid reasons to seek care.
Seeing a provider doesn’t just mean getting medication. Today’s pain management strategies include lifestyle modifications, physical therapy, targeted procedures, and holistic approaches tailored to your specific symptoms and health goals. The sooner you reach out, the sooner you can start feeling better.
Conclusion
Chronic pain is a complex condition that affects both the body and mind, often creating a mix of physical symptoms, emotional strain, and functional limitations. Understanding the different sensations, physical signs, and secondary effects is the first empowering step toward effective chronic pain management.
You don’t have to navigate chronic pain alone. Reaching out for help opens the door to real relief, better function, and a higher quality of life.
Frequently Asked Questions
-
The most common and defining symptom is persistent pain lasting longer than three months. This discomfort may be constant or come and go in cycles, but it never fully resolves. The pain can feel aching, sharp, burning, or throbbing depending on the underlying cause.
-
Pain may be chronic if it continues beyond the normal healing timeframe, frequently returns, or interferes with daily activities such as sleep, mobility, or work. Chronic pain often persists despite rest, medication, or self-care efforts. Tracking your pain pattern and frequency can help you identify whether it’s becoming long-term.
-
Chronic pain can lead to measurable physical changes such as stiffness, muscle tension, tenderness, inflammation, and reduced range of motion. Secondary effects may include fatigue, sleep problems, weakness, or postural changes as the body adapts to ongoing discomfort.
-
Daily chronic pain management may include:
Gentle movement or stretching
Heat/ice therapy
Mindfulness and stress-reduction techniques
Proper sleep hygiene
Over the counter or prescribed medications
Physical therapy or targeted exercises
Consistent hydration and nutrition
A personalized treatment plan is ideal, especially when symptoms fluctuate or worsen over time.
-
Yes. Long-term pain activates the body’s stress response, which can impact immune function, increase inflammation, and make you more vulnerable to illnesses. Poor sleep, fatigue, and stress all common in chronic pain further influence immune health.
-
You should seek medical care if your pain lasts longer than three months, disrupts daily life, worsens over time, or doesn’t improve with self-management. Warning signs such as numbness, tingling, weakness, swelling, fever, or radiating pain should also prompt a professional evaluation. Chronic pain is a medical condition you never need to “tough it out.”